Frequently Asked Questions
-
What is the atmosphere between staff physicians and Residents?
Residents work one-on-one with the many staff physicians in the management of all private patients. The staff are extremely eager to work with residents and to involve the residents in all aspects of patient care. Once a patient has delivered or had surgery, it is the responsibility of the resident to manage the hospital course of these patients under the direct supervision of the attending staff. This allows the residents to experience a diverse approach to patient care. We take pride in offering a variety of training backgrounds.

-
What is the volume of High Risk Obstetrics?
All high-risk obstetric patients are closely followed and staffed by a board-certified Maternal-Fetal Medicine Specialist. Our prenatal assessment center cares for patients with a wide variety of medical conditions, including diabetes, hypertension, and heart disease. In addition, all OB/GYN residents rotate through the High Risk Obstetrics service during their second and third year. By the end of the residency training, all residents are proficient in obstetrical ultrasound.

-
How much cesarean, forceps and VBAC experience do the residents receive?
The residency is fortunate to have many staff skilled in the application of forceps and vacuum. By the end of residency, all residents feel comfortable with the application of forceps under appropriate circumstances.

-
What teaching responsibilities do the residents have?
Ascension Wisconsin is dedicated to the education of its residents and to the medical students who rotate on campus. Third year students from Medical College of Wisconsin and Idaho College of Osteopathic Medicine spend 4-6 weeks on the OB/GYN rotation. We also host senior medical students who are interested in further training in Obstetrics and Gynecology. Residents also teach Family Medicine residents clinical concepts on labor and delivery and in the clinic.

-
Is there a research requirement?
Residents are required to participate in scholarly activity as part of their residency education.
Each spring, we conduct a Resident Research Day program where PGY-3&4 residents present clinical research using available clinical data under sponsorship of clinical faculty/staff. PGY-4 residents facilitate presentations and discussion. Our program financially supports research initiatives; and there is a full-time statistician as part of the GME office.
-
Do the residents have their own continuity clinic?PGY-1-3 residents have a continuity clinic. In this setting, residents see their own panel of patients under the supervision of an attending once a week. Residents are encouraged to deliver and perform surgeries for their continuity patients.
.jpg)
-
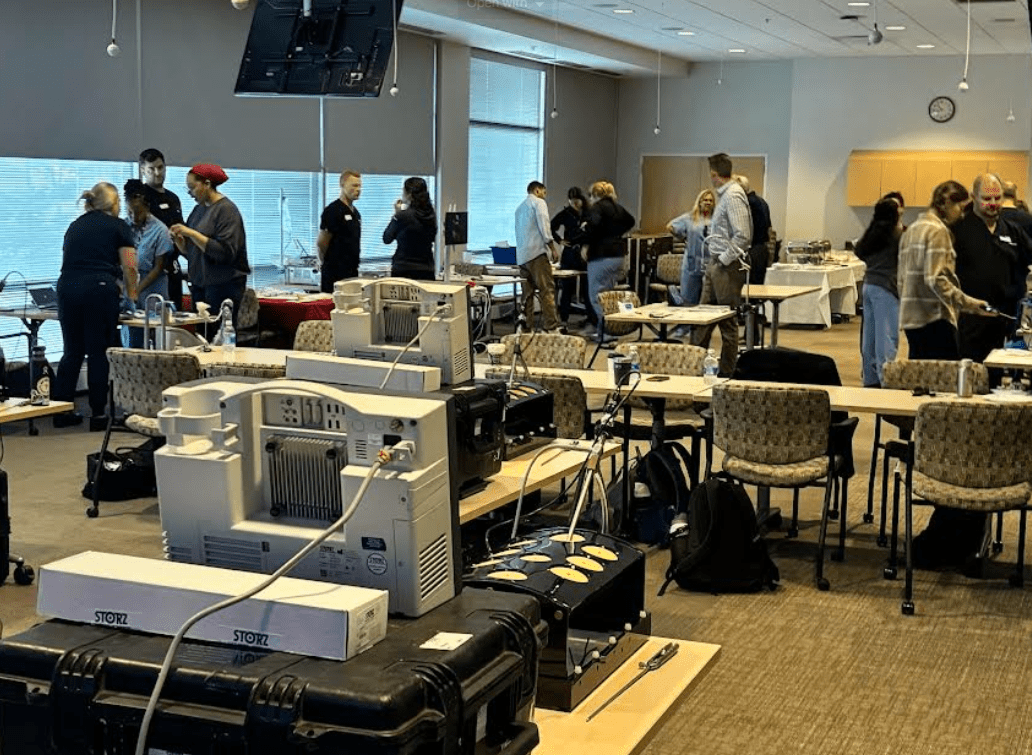
What type of didactic sessions are there?
Wednesday afternoons are specifically set aside for didactic sessions. Residents are excused from all other responsibilities to attend these mandatory education sessions. Our faculty host a series of lectures, simulations and conferences that will provide in-depth education on obstetrics and gynecology. We have regularly scheduled journal clubs, M&M and Pathology conferences. Approximately once a quarter [Fifth Wednesday], we also have a health & wellness curriculum.
-
Does all residency training take place in one facility?
The majority of resident rotations occur at either Ascension St. Joe’s and Columbia St. Mary’s. These facilities are all within 6 miles of each other and easily accessible by car. Throughout the resident’s four years of training, there are offsite rotations designed to maximize educational experiences.
