AMBULATORY CARE Post-Graduate Year 2 Pharmacy Residency
AMBULATORY CARE PHARMACY RESIDENCY PROGRAM OVERVIEW

Residency Focus
Program Site Description
Purpose Statement
AMBULATORY CARE PRACTICE SITES
The PGY-2 ambulatory care resident will have the opportunity to practice at a variety of ambulatory care practice sites. The two primary patient care sites for required longitudinal learning experiences are the St. Vincent Joshua Max Simon Primary Care Center and St. Vincent Medical Group patient-centered medical home sites. Information about the required and elective practice sites are listed below.
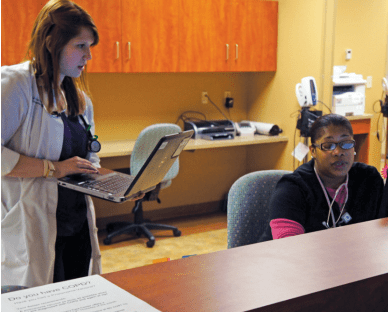
St. Vincent Joshua Max Simon Primary Care Center (PCC): The PCC is a medical residency training facility where physicians provide optimal outpatient care to a diverse patient population including multiple patient languages and varying degrees of health literacy. This facility includes Internal Medicine, Family Medicine, OB/GYN, and Pediatric clinics as well as a variety of sub-specialty clinics. The pharmacists provide collaborative drug therapy management to adult patients for a variety of disease states and have direct patient care coverage responsibilities for the Internal Medicine and Family Medicine clinics. An on-site pharmacy provides unique services to this uninsured and underinsured patient population. The Primary Care Center is located on the St. Vincent Indianapolis campus.
Ascension Medical Group of Indiana (AMG): The Ascension Medical Group of Indiana includes over 500 medical providers located throughout the state, many of whom are working to practice in the patient-centered medical home model. Pharmacy services expanded into the patient-centered medical home sites in 2016, providing collaborative drug therapy management and population health initiatives. The goal is to continue to expand pharmacy services to additional SVMG sites over the next several years with the hope of implementing telehealth services for more rural locations.
St. Vincent Medication Management Services Anticoagulation Clinic (MMS): MMS is a hospital-based outpatient clinic providing pharmacist-driven anticoagulation services. In addition to providing anticoagulation management, MMS provides medication management services, post-discharge diabetes education, and immunizations to enrolled patients. MMS has also provided immunization services to a variety of organizations and corporations within central Indiana. MMS has 3 locations in Central Indiana- Indianapolis, Carmel and Fishers hospital campuses.
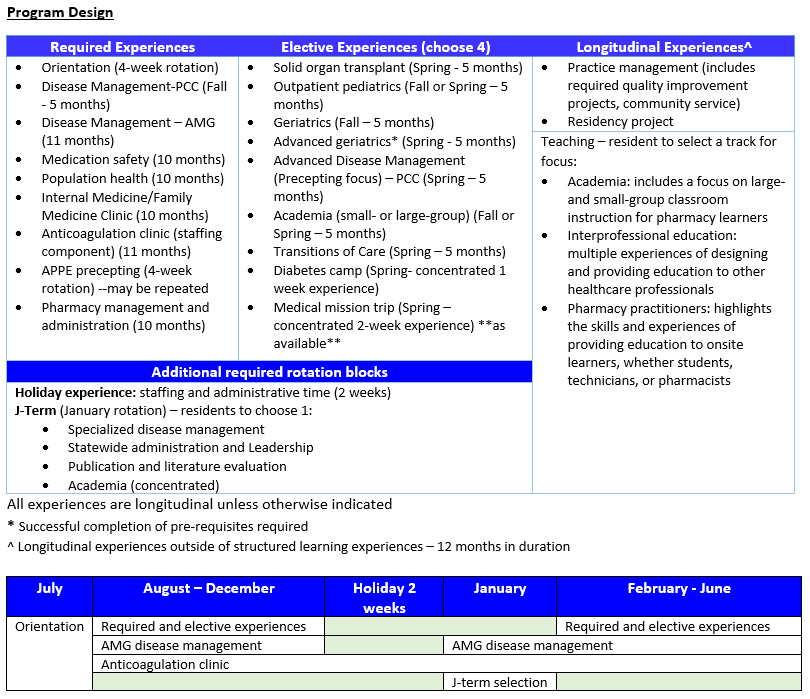
Program at a glance

Longitudinal Learning Experiences
Medicine Experience:
The Medicine Experience will incorporate the resident Family Medicine (FM) and Internal Medicine (IM) clinics, and is designed to provide the resident with the foundational knowledge about common acute/chronic disease state management of adults and children through direct instruction, observation and modeling by the preceptors. Residents will have the opportunity to apply this knowledge through participation in multidisciplinary patient care at the St. Vincent Joshua Max Simon Primary Care Center (PCC), working with various healthcare providers in managing social and medical aspects of total patient care.
Activities include:
- Daily patient chart review and care plan development
- Adherence evaluations and medication histories
- Provide drug information resources and pharmacotherapy
- Participate in transitions of care medication treatment recommendations to medical residents and staff reconciliation
- Patient/provider education and optimal medication management
Collaborative Drug Therapy Management:
The longitudinal Disease State Management experience is designed to provide the resident with the foundational knowledge of pharmacy-driven clinics for the following disease states (adult focus): anticoagulation, asthma, COPD, diabetes/pre-diabetes, heart failure, hyperlipidemia, hypertension, immunizations, medication therapy management, and tobacco cessation. The resident will be responsible for providing care to patients per the Collaborative Drug Therapy Management (CDTM) practice agreement two half days per week throughout the year and will document all activities within the electronic health record. The resident will participate in ongoing outcomes-based research by evaluating the outcomes of these pharmacy-driven disease-state management of clinics, as well as participating in the annual review and revision of the CDTM individualized disease state protocols.
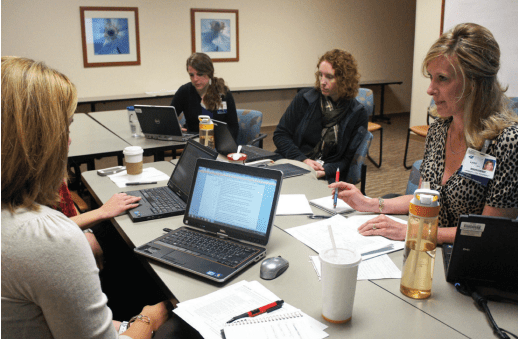
Practice Management:
The Practice Management longitudinal experience is designed to provide the resident with the foundational knowledge about the medication use process, practice management skills, medication safety, and medical informatics through participation in hospital and clinical committees. The resident will be given dedicated administrative time to fulfill practice management expectations throughout the residency. Activities include, but are not limited to:
- Publication preparation and submission
- Quality improvement/ benchmarking projects; drug class reviews
- Prior authorization approvals
- Wellness initiatives
- Formal drug information questions
- Professional development activities
- Development of new service or evaluation of an existing service
Population Health, Quality Management, and Medication Safety:
These experiences is designed to provide the resident with the knowledge and experience to participate in improving patients’ care using population data and quality metrics. The resident will participate in and design a variety of initiatives aimed at improving the overall quality and cost-effectiveness of the care of patients at specified practice sites. In addition, the resident will participate in activities and initiatives designed to improve the culture of medication safety, to evaluate and respond to medication safety reports, and to evaluate and decrease risk prospectively. As part of the teaching component, the resident will work with preceptors and the Community-based PGY1 pharmacy residents to develop the 6th annual medication safety escape room for the medical residents.
Teaching / Education Experiences
Residents will have the opportunity to provide a variety of teaching/lecture experiences at St. Vincent Indianapolis as well as other ambulatory care practice sites. They will have the opportunity to mentor PGY-1 pharmacy residents and pharmacy students, and participate in elective academia based teaching experiences at Butler University College of Pharmacy and Health Sciences (COPHS), Manchester University College of Pharmacy and Purdue College of Pharmacy. Additionally, the resident will participate in the Indiana Pharmacy Resident Teaching Certificate (IPTeC) Program through Purdue and Butler universities, if not already completed.
Residents have the option of participating in teaching experiences for many different audiences and groups of learners, both in the classroom and in practice. Alternatively, residents may choose to select a teaching track, enabling them to focus on provision of teaching to a more focused group of learners. Track options include pharmacy academia, inter-professional education, and pharmacy practitioners and experiential learners.
Teaching activities may include:
- One-hour didactic lectures. Audience may include pharmacy staff, medical providers, pharmacy students, or other healthcare professional students.
- One didactic lecture must be an Outpatient Pharmacy Grand Rounds for the statewide outpatient pharmacy team, regardless of chosen track.
- Inter-professional education opportunities geared toward support staff – Formal presentation or written (i.e. newsletter)
- Serving as co-preceptor for pharmacy students during clinic activities and primary preceptor for one pharmacy student rotation during the second six months of the residency experience.
- Facilitating monthly student standing topic discussions
- Providing monthly PGY-2 topic discussion from prespecified topic list
- Completing a minimum of three preceptor development activities as made available by the preceptor development committee
- Providing a pharmacy-focused quarterly newsletter for primary care providers
- Electronic medication safety communications (social media, interactive games)
- Interactive didactic presentation (the medication safety escape room)
Residency Project
Staffing Commitment
PGY-2 AMBULATORY CARE PAST RESIDENTS – WHERE ARE THEY NOW?
Lauren Turner, PharmD, is an ambulatory care clinical pharmacist at Community Health Network in Indianapolis. Her resident project evaluated safe prescribing of DOACs in an outpatient population.
Nicole Jasperson, PharmD, is an ambulatory care clinical pharmacist with Community Health Network in Indianapolis and an adjunct faculty with Purdue University. Her resident project involved evaluation of prescribing practices in poorly controlled hypertensive patients.
Stephanie O’Brien, PharmD, is a co-funded ambulatory care pharmacist with the University of St. Joseph School of Pharmacy, West Hartford, CT. Her resident project investigated unmeasurable doses prescribed to pediatric patients who are discharged from the NICU to the outpatient setting.
Jessica McKinney, PharmD is an ambulatory care clinical pharmacist at Community Health Network in Indianapolis. Her research project evaluated clinical outcomes in a pharmacist-run disease state management clinic.
Alana Juodvalkis, PharmD, BCACP is an ambulatory care clinical pharmacist at ___. Her resident project evaluated patient satisfaction and clinical outcomes with drive-up anticoagulation pharmacy visits.
Olivia Craker, PharmD is an ambulatory care clinical pharmacist with Ascension St. Vincent in Indianapolis. Her research project assessed prescriber understanding and usage of pharmacogenomic testing in the primary care setting.
PRIMARY PRECEPTORS FOR THE SPECIALTY RESIDENCY IN AMBULATORY CARE





Deborah Zeitlin, PharmD, is an Ambulatory Care Clinical
Pharmacist and an Associate Professor of Pharmacy Practice at Butler University
College of Pharmacy and Health Sciences. She received her Doctor of
Pharmacy from Butler University. She went on to complete a PGY-1
residency at Medical College of Virginia Hospital in Richmond, Virginia and a
PGY-2 residency in Ambulatory Care at University of Illinois at Chicago in
Chicago, Illinois. Her interests include anticoagulation, chronic disease
state management, self-care management, and academia. She enjoys working
with learners in all settings.

